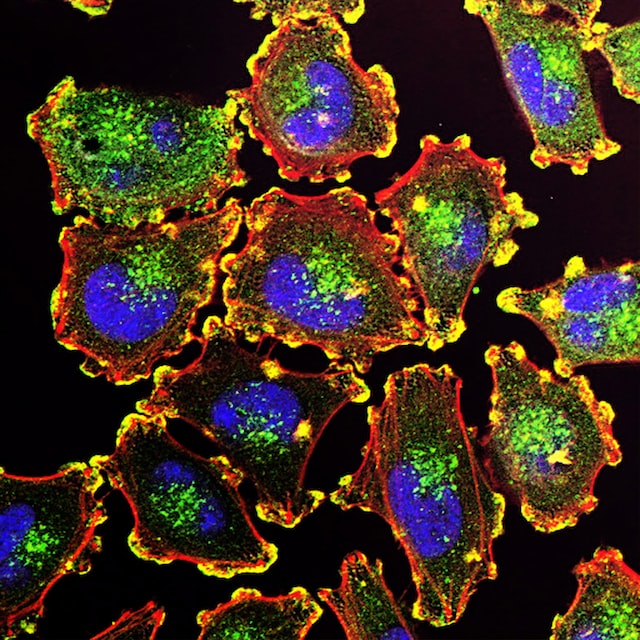
With the advancement of oncology research, oncology therapies are becoming more and more diverse, and immunotherapy has gradually become a research hotspot in recent years. Chimeric Antigen Receptor T Cell (CAR-T) is a type of cell therapy in which T cells isolated from patients or allogeneic donors are genetically engineered to express chimeric antigen receptors to specifically identify and kill tumour cells.

To date, CAR-T has made significant breakthroughs in the treatment of a variety of relapsed or refractory haematological tumours, but breakthroughs in the treatment of solid tumours have been difficult to achieve. For this reason, researchers around the world are constantly working to develop effective CAR-T therapies for solid tumours.
Recently, Science published two consecutive research articles proposing new ways to improve the efficacy of CAR-T for solid tumours. The two studies, each based on a synthetic biology strategy, provide a new upgrade to CAR-T cells to enhance the immune response induced by CAR-T cells against diseased tissue, demonstrating how synthetic biology can be used to address a difficult problem in cancer immunotherapy.
On 15 December, Science published a paper entitled "Multidimensional control of therapeutic human cell function with synthetic gene circuits". In this study, Boston University's A. B. H. A., a researcher in the field of immunotherapy, has published a paper entitled "Multidimensional control of therapeutic human cell function with synthetic gene circuits. In this study, a team led by Professor Ahmad Khalil at Boston University developed a toolkit of 11 programmable synthetic transcription factors that can be activated on demand by the timed administration of FDA-approved small molecule inducers. Using these tools, the researchers engineered human immune cells that can activate specific cellular programs, such as proliferation and anti-tumour activity, on demand.
The researchers tested the in vivo efficacy of synZiFTR-regulated CAR-T cells using a simple xenograft blood tumour model and showed that the synZiFTR circuit can be used to program drug-dependent, post-delivery control of T cell anti-tumour activity in vivo. In addition to controlling CAR-mediated tumour targeting, synZiFTR is also suitable for controlling the expression of other proteins, such as IL-2 or Il-12, and the regulation of these cytokines represents a safer way to exploit them to enhance the efficacy of immune cells.
To establish a proliferative gene switch, the researchers used TMX-inducible synZiFTR to regulate super IL-2 expression, effectively providing dose- and time-dependent control of therapeutically relevant genes in vivo and in vitro.
In summary, with this study, the researchers have designed and tested a clinically inspired set of synthetic gene regulators and circuits in human cells with some therapeutic potential.
In a separate study published in Science on 16 December, a team of researchers from the University of California, San Francisco used a recently developed synthetic Notch receptor to design enhanced CAR-T cells with a second receptor that recognises tumour antigens and subsequently leads to the release of the cytokine interleukin 2 (IL-2) from T cells. In a mouse model, this approach enabled the infiltration of CAR-T cells into solid pancreatic and melanoma tumours, leading to the eradication of a large number of tumours. The research paper is titled "Synthetic cytokine circuits that drive T cells into immune-excluded tumors".
A variety of solid tumours do not respond to T-cell therapy because their immunosuppressive microenvironment prevents T-cell infiltration, activation and proliferation, and the main tumour suppression mechanisms include inhibition of T-cell receptor signalling and depletion of inflammatory cytokines. On this basis, overcoming the suppressive tumour microenvironment is a major obstacle to immunotherapy of solid tumours.
Supplementing T-cell activity with inflammatory cytokines (e.g. high doses of IL-2) can drive effective anti-tumour function, but systemic IL-2 treatment can cause serious adverse effects. Autonomous cytokine production has the potential to overcome toxicity by direct local delivery of cytokines to tumours, and researchers have designed therapeutic T cells with synthetic cytokine circuits in which tumour-specific synthetic Notch (synNotch) receptors drive IL-2 production. These tumour-targeting IL-2 delivery circuits offer a potential way to overcome local tumour suppression while minimising systemic IL-2 toxicity.
The researchers observed that engineered synNotch→IL-2 inducible circuits drove chimeric antigen receptor or TCR-T cells to efficiently infiltrate immune exclusion tumour models of pancreatic cancer and melanoma. In these challenging immunoreactive tumour models, significantly improved infiltration was associated with tumour clearance and survival. Unlike systemically delivered IL-2, the local cell-based IL-2 circuit did not show toxicity as the synNotch→IL-2 circuit was not dependent on TCR/CAR activation, but was still tumour-targeted.
Immunoassays showed that CAR-T cells expanded only within the tumour, with increased markers of activation and decreased markers of failure. Synthetic IL-2 production allows infiltrating T cells to survive and initiate sustained CAR-mediated activation, expansion and tumour killing. These modified T cells appear to act as pioneers, triggering tumour expansion through their synNotch-induced IL-2 production, which then synergistically initiates sustained CAR/TCR-mediated T cell activation and killing. This type of synthetic cytokine delivery circuit could provide a powerful and versatile approach to remodelling and overcoming immunosuppressive solid tumours.
The above findings suggest that it is possible to reconfigure T-cell circuits to re-establish the critical outputs required for a robust anti-tumour response, but in a manner that bypasses key points of tumour immunosuppression. These types of engineered local cytokine delivery circuits may therefore provide a potentially versatile strategy for driving effective T cell activity against immunosuppressed solid tumours.
In the above two studies, two research teams have proposed strategies in which the use of synthetic genetic circuits could better control the timing of immunotherapy, allowing for on-demand activation of anti-tumour cell function. These studies are not limited by natural immunology, but rather expand the range of immune responses triggered by CAR-T cells against diseased tissues, offering some hope for hard-to-treat solid tumours.